M.S. Capstone Project | Spring, 2025 | Role: UX Researcher and Designer
Table of Contents
Introduction
In this semester-long Capstone project, I explored opportunities to redesign the mHealth experience of veterans with PTSD transitioning out of the military.
I focused on three things:
- Developing AI conversational patterns for normalizing discussion of trauma.
- Designing an identity-affirming UI system.
- Creating culturally appropriate user interactions that support stigma-reduction and treatment seeking.
To execute this project, I followed an interdisciplinary design approach combining user-design methods with clinical and psychological research in a veteran-centric design process. I developed several research deliverables, including user journey and storyboards, to visualize and communicate design opportunities. I translated insights into working prototypes to demonstrate viability of new design patterns and interaction models, leveraging advances in conversational and explainable AI.
Design Challenge
While mHealth tools in the mental health space are plentiful, they are often designed from a clinical perspective and miss out on cultural nuances that shape experiences and use over time. One problem with these tools is that they view veterans as generic users with generic needs. In this project, I focused on veteran identity as a jumping point for exploring novel interactions and uses of emerging tech in the mental health space.
Why It Matters
Research has shown that posttraumatic stress disorder (PTSD) is disproportionately common among veterans, reflecting historical patterns that continue despite greater acceptance and understanding of mental health. Moreover, when veterans transition from the military, they are separated from their support networks and have difficulty coping with mental health problems on their own.
While Veterans Affairs (VA) mental health services provide some care, they continue to be underutilized by veterans due to continued stigma against mental health and help seeking in the military.
Design Outcomes
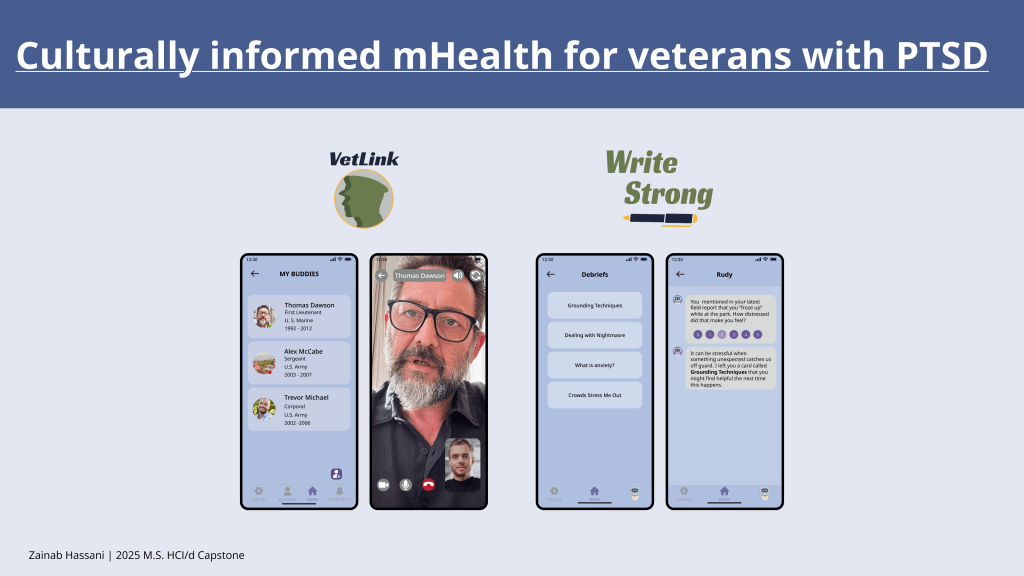
I developed UI and UX patterns to normalize talking about trauma during the early homecoming phase by:
- Leveraging conversational AI for progressive disclosure of coping strategies and other clinical resources.
- Facilitating peer-to-peer interactions with mentors in a social network.
- Supporting mental health journaling and integrating AI analytics to perform mental health diagnostics.
How Might We Bridge the Trauma Divide?
Destigmatizing PTSD and educating veterans through peer support and AI-supported journaling.
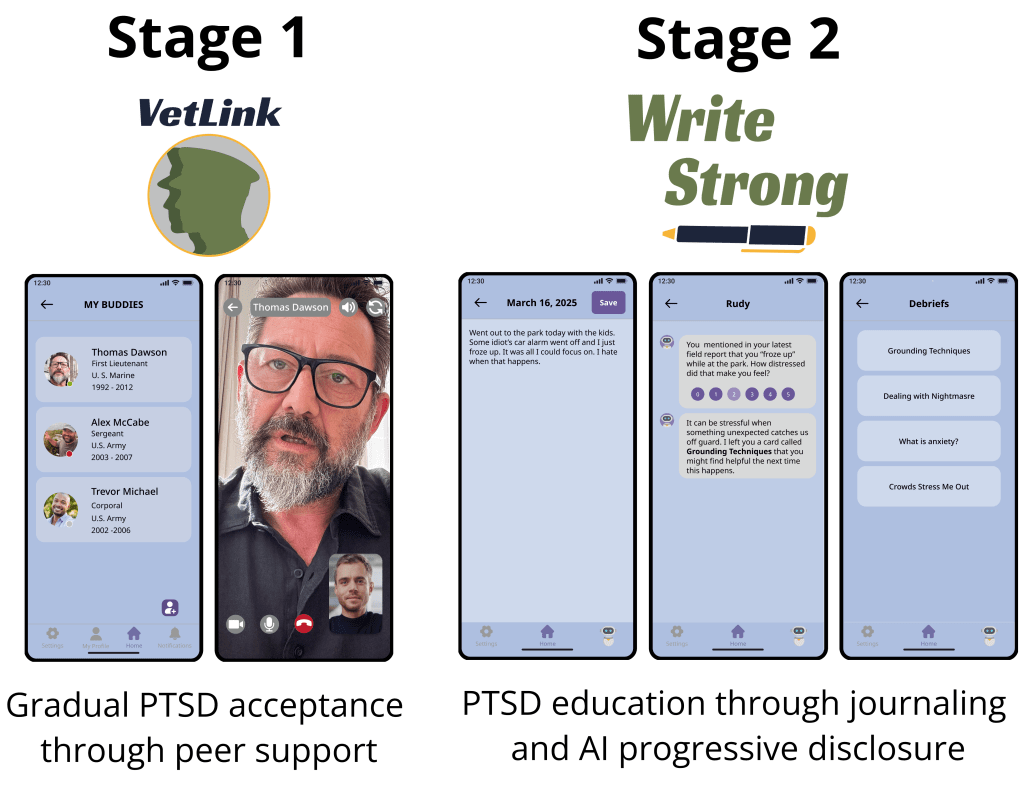
We can bridge the trauma divide through a two-stage process that uses peer support and an AI-supported journaling intervention to gradually normalize PTSD for the veteran while also educating them about trauma and coping strategies.
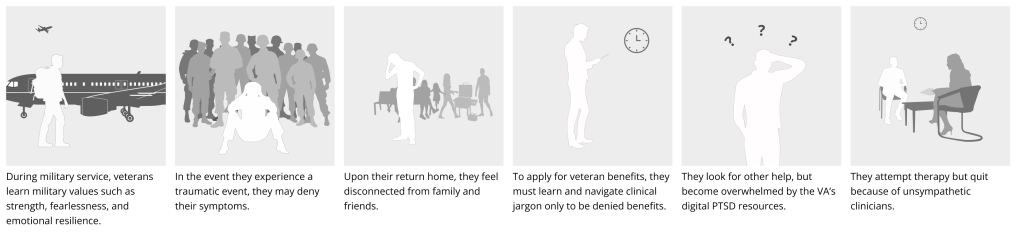
The process could look like the storyboard presented below.
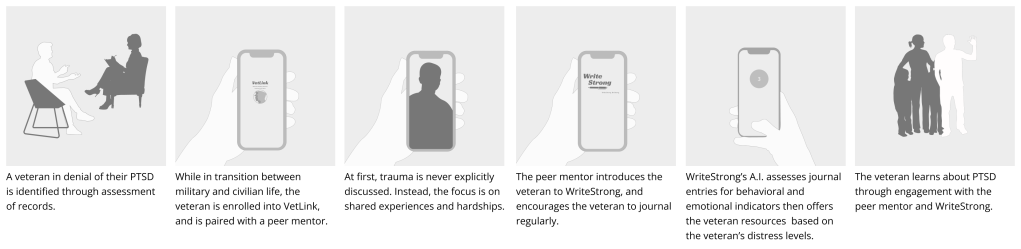
A storyboard showing what the veteran experience may look like through this proposed normalization process.
PTSD Denial Identification Through Machine Learning
When completing mental health assessments as part of standard military separation procedure, veterans with PTSD may not give honest answers. However, the metrics below can be used in combination to assess the likelihood that a veteran has PTSD and is in denial.
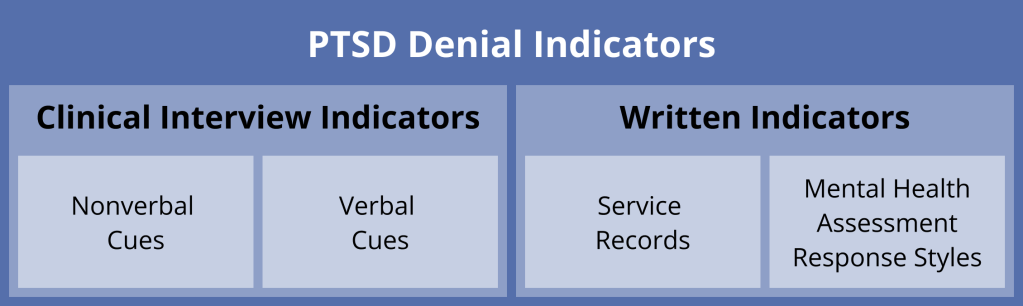
The combination specific indicators can be used to determine the likelihood that a veteran has PTSD and is in denial of their symptoms.
Machine learning can be used to holistically analyze these factors and determine the likelihood that a veteran is experiencing posttraumatic symptoms.
PTSD Destigmatization through Peer Support
Eligible veterans are enrolled into the VetLink peer support program, where they’re paired with a mentor who has also experienced PTSD while in the service. They’re also encouraged to add their own friends and family as contacts to help them recognize their existing support network.
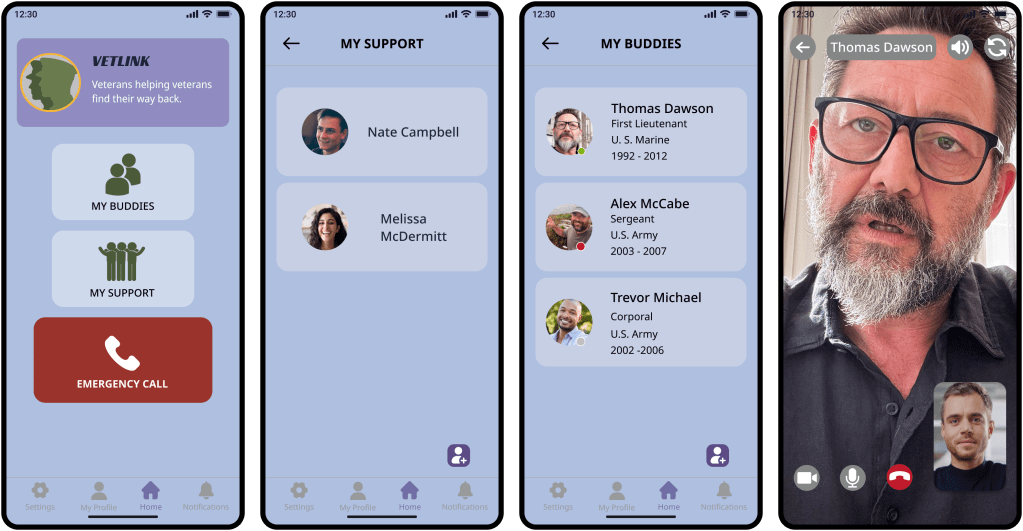
VetLink connects veterans to peer mentors to gradually help them accept their trauma and promotes the recognition of their existing support system.
The mentor gradually shares their own experience with PTSD. This behavior modeling will help the veteran reflect on their own experience, accept their PTSD, and encourages them to seek formal support.
Why Destigmatization through Peer Support?
- Veterans prefer to socialize with those who have gone through similar experiences as them.
- Peer support from veterans who have experienced trauma reduces PSTD stigma among veterans.
Progressive Information Disclosure Through AI Assisted Journaling
During the early stages of transition, the peer mentor introduces the veteran to the WriteStrong journaling app, and encourages them to write regularly. Veterans can either write free form or answer a daily prompt.
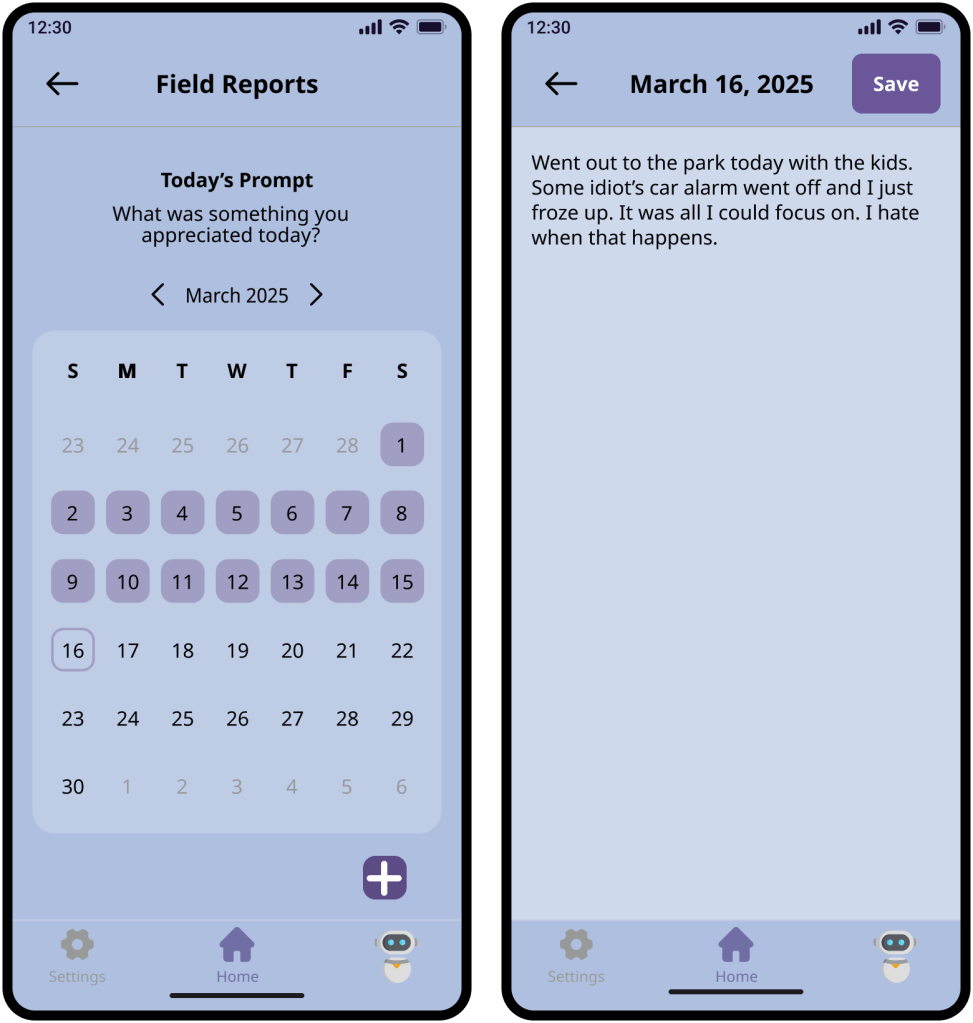
Veterans can either answer a prompt or write freeform journal entries.
WriteStrong’s AI analyzes journal entries and looks for cues indicative of a traumatic reaction.
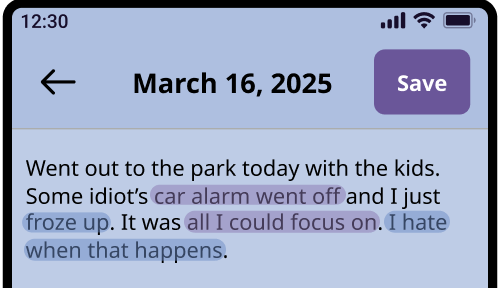
WriteStrong’s AI evaluates journal entries for language that may indicate that the veteran had a traumatic response to a situation.
If the AI suspects that the veteran experienced a posttraumatic reaction, the AI will ask the veteran to indicate what level of distress they felt in that moment, and recommend resources based on the veteran’s answer.
| Distress Level | Resource Recommendations |
| 0 – 1 | None |
| 2 | Debriefs |
| 3 | Online Resources (AboutFace, MaketheConnection) |
| 4 – 5 | VA Mental Health Referral |
A table representing how the AI will respond based on the veteran’s subjective level of distress.
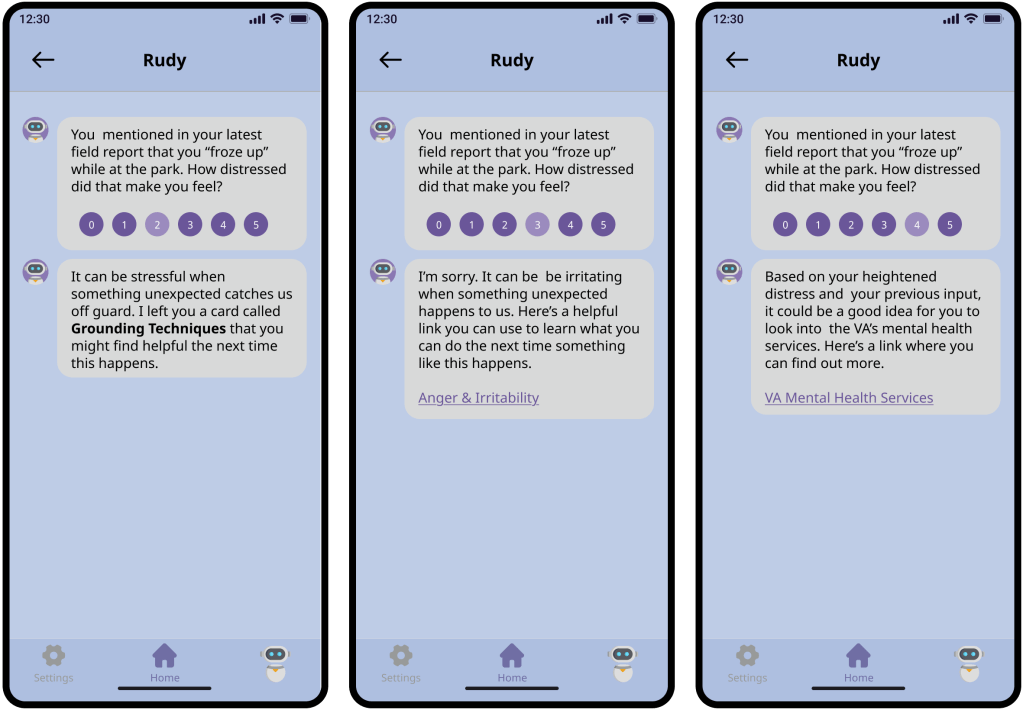
Example of how the AI might respond to the veteran.
Why AI Progressive Disclosure?
- Inadequately trained or impatient mentors could disclose information at inappropriate times or not at all.
- Peer mentors may not be adequately equipped to answer the veteran’s questions or provide information.
- If the mentor is the one delivering information and tools to the veteran, the burden of doing so would fall on them and create mentor stress.
- Having information about mental health or trauma visible to the veteran right off the bat could further stigmatize veterans already struggling with denial.
- Providing the veteran with pre-made information cards and existing online resources ensures that the veteran is given accurate information.
Design Process
Mapping the Ecosystem
Ecosystem mapping consisted of a series of interconnected activities:
- Secondary research
- Online artifact analysis
- VA Journey map analysis
- Clinician expert interviews
To learn about veterans’ lived experiences, I analyzed posts and comments made by veterans on veteran-focused Reddit communities and examined veterans’ stories on MaketheConnection, a VA-affiliated website that seeks to destigmatize PTSD by sharing veterans’ stories. I also analyzed publicly available journey maps created by the Veteran Experience Office to educate myself about the veteran’s experience transitioning from the military to civilian life and navigating the VA claims process.
The Application Process
I began by familiarizing myself with the traumatized veteran’s ecosystem. Through my initial research, and by analyzing Reddit posts, I constructed a diagram representing what happens when the traumatized veteran applies for VA benefits.
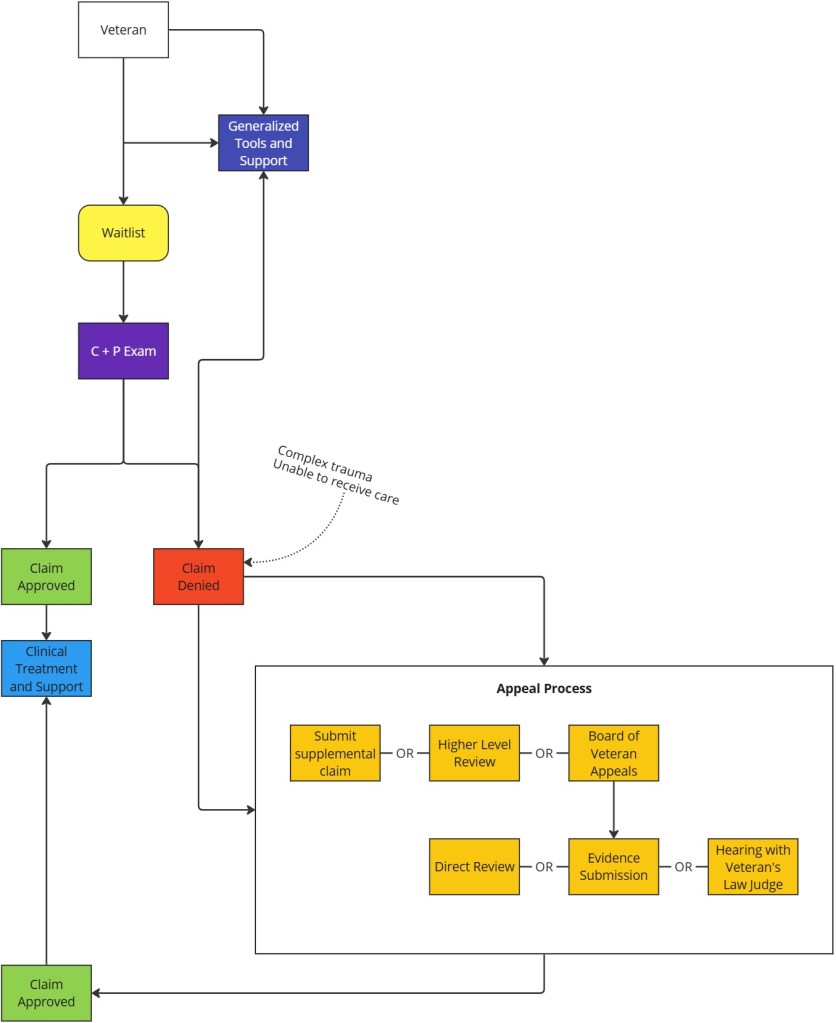
A diagram representing what happens when a veteran with PTSD tries to apply for VA benefits.
As demonstrated, there are two types of veterans: those who can easily get through the VA system and get help, and those who cannot. While valid reasons exist for VA claim denial, we can determine a predictable pattern when considering the stigmatized veteran’s experience.
Veterans in denial of their symptoms often face challenges when applying for veteran benefits.
But why does this pattern exist in the first place?
Discovering Themes Through Affinity Mapping
To answer that question, I used affinity mapping to organize my insights, and uncovered the following themes.
- A need for support networks
- Inconsistencies and stressors in the claims process
- Stressors related to treatment
- The role of military culture and stigma
- Lack of understanding and clarity about process and benefits
Examining the sub-themes within these larger thematic umbrellas, I developed an ecosystem map representing the different barriers faced by veterans.
Veteran Affairs
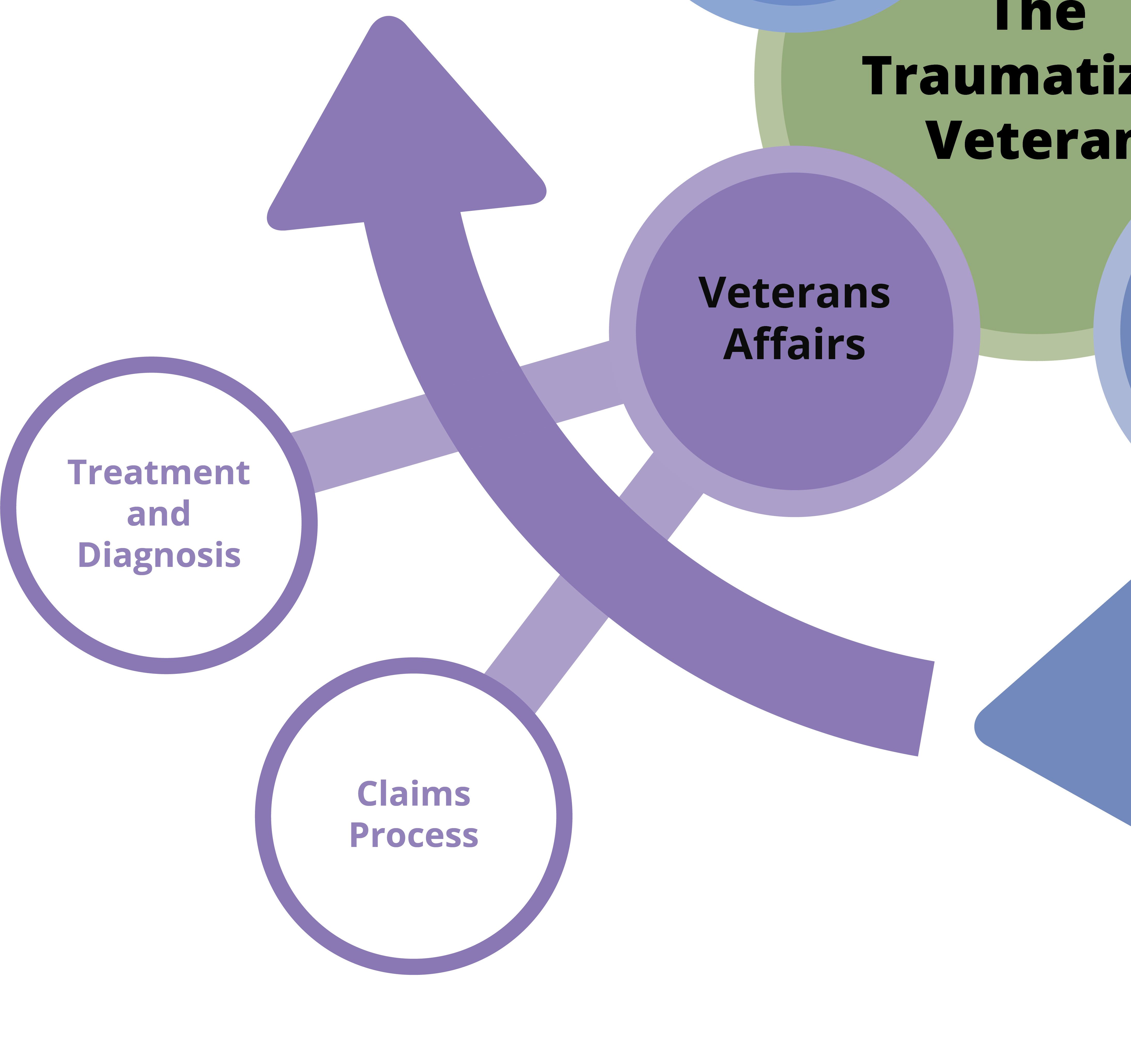
VA-related factors impacting the stigmatized veteran experience can be described as the following:
- Treatment-focused professionals may not understand the difficulties of veterans with PTSD.
- Demonstrating service connection can be difficult when the connection between trauma and service is ambiguous or the trauma complex.
- Needing veterans to constantly describe their trauma can retraumatize them, and isn’t feasible for those veterans who have difficulty recalling the exact details of their trauma.
Military Culture
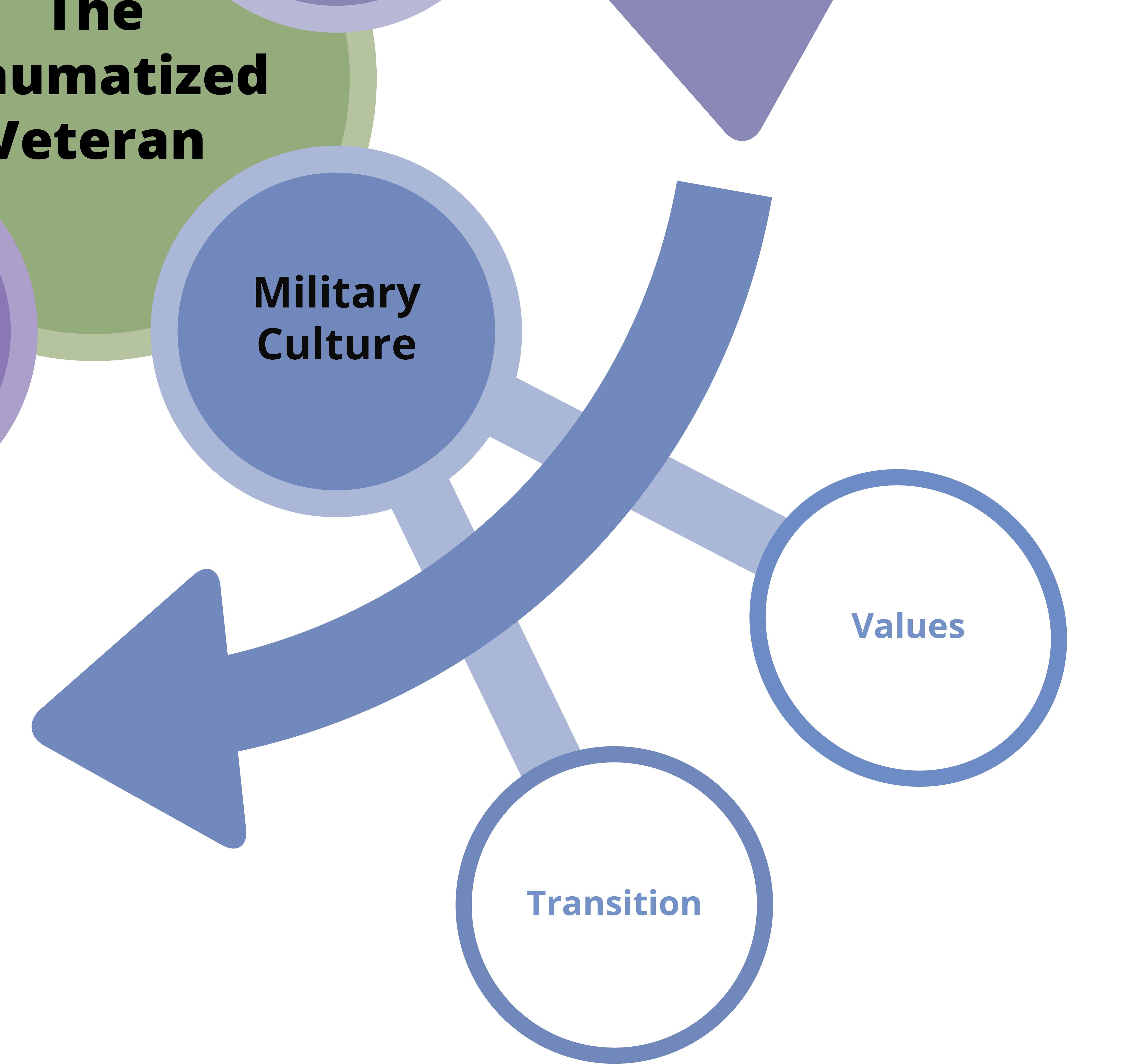
Joining the military means being immersed in that unique culture and embodying their values.
Military values and cohesion combine to the veteran’s struggle with PTSD.
Similarly, because teamwork and group cohesion are key components to the military unit, any sign of weakness within the group risks unit success.
The bonds made through deployment strengthen as the veteran’s service continues. However, all the support and connections the veteran had during their deployment abruptly disappears when they separate from the military.
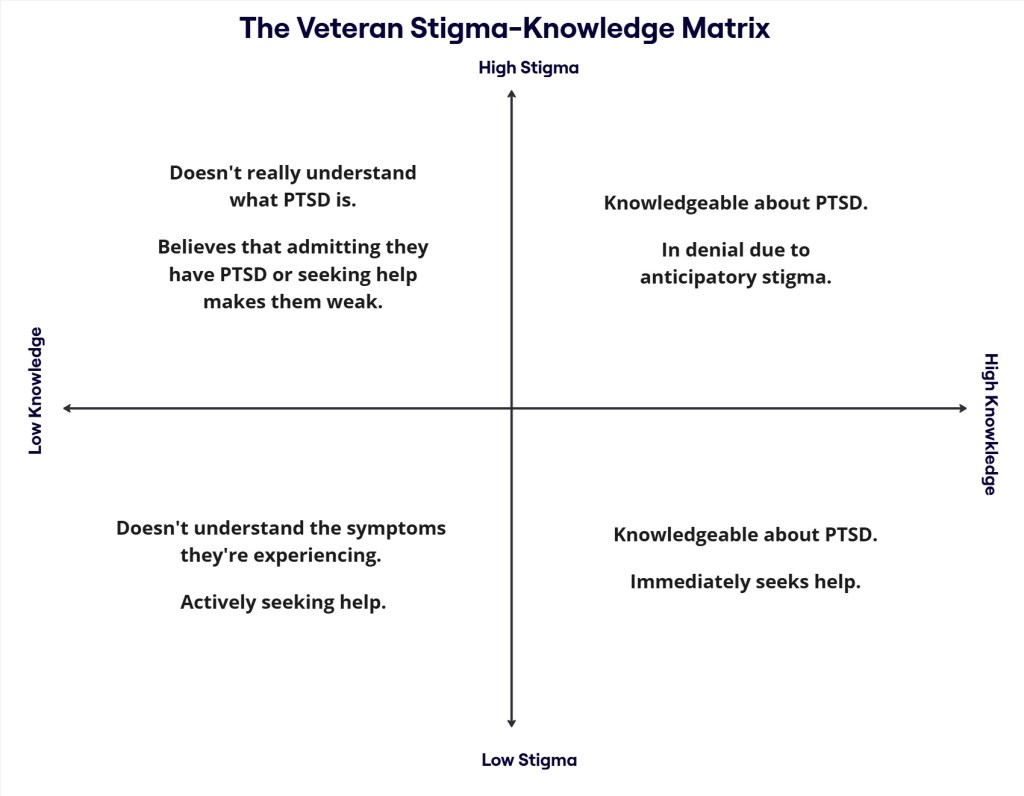
Stigma
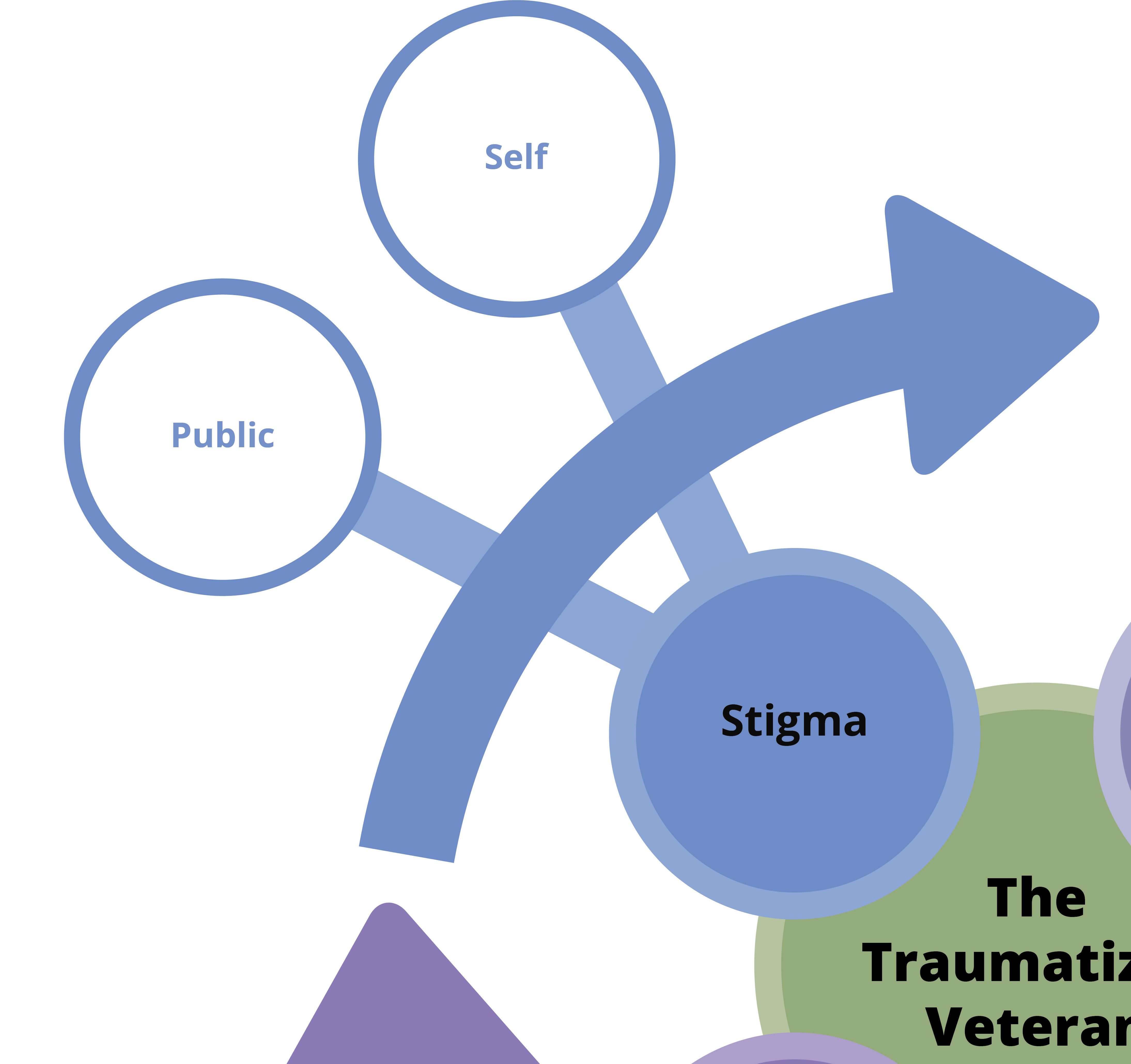
Stigma and military culture are interconnected factors that mix to create the circumstances in which the veteran denies their trauma.
However, PTSD knowledge can be visualized as a matrix.
A matrix representing the relationship between stigma and PTSD knowledge.
This diagram reflects two types of stigma. Public stigma (society’s negative beliefs about a group) and self-stigma (how someone internalizes society’s negative beliefs).
After consulting with a clinical expert on this topic, I learned three additional insights:
- Self-stigma impacts veterans the most.
- Veterans need social support to help them thrive.
- While veterans do learn about VA services while transitioning out, a traumatized veteran experiencing stigma is unlikely to be receptive to that information.
Information
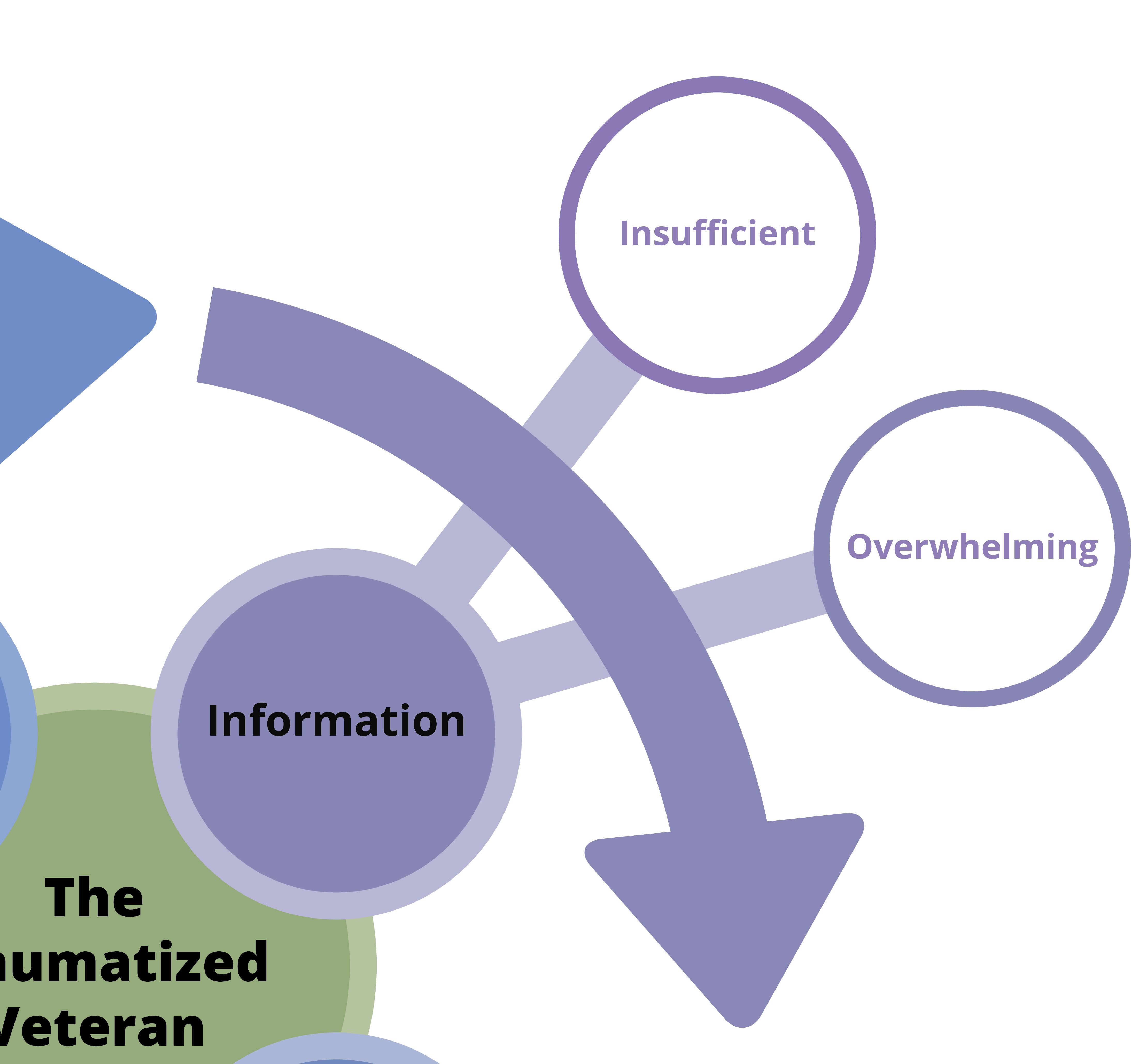
When seeking treatment or information about PTSD, veterans are simultaneously given too much and too little information. For example:
- Veterans filing for VA benefits are frustrated by the steps involved, and the clinical jargon used throughout the process.
- Lack of guidance leads to veterans seeking out third party sources to fill in the gaps. Consequently, veterans may mistakenly assume that veteran anecdotes represent a universal experience.
- The VA does provide veteran-centric PTSD resources, but it can get buried or be difficult to find because these resources are geared towards a general audience.
For a more in-depth analysis of how the veteran experience is impacted by the problem of information, you can check out my Medium article.
Putting It All Together
The Veteran’s Ecosystem
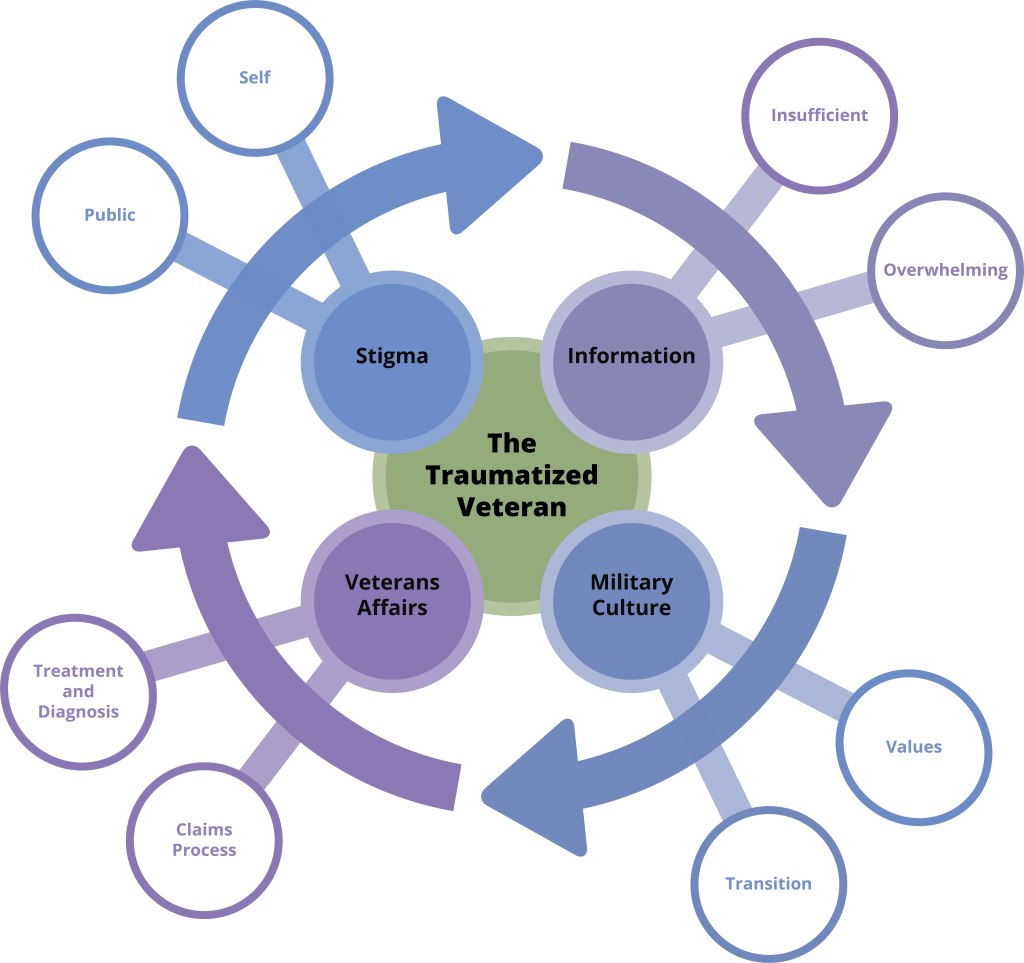
The veteran’s experience is shaped by an ecosystem consisting of many interconnected factors.
When we zoom out, we see the veteran experience as an interconnected landscape, impacted by several interrelated factors.
But what exactly does this experience look like?
Journey Mapping
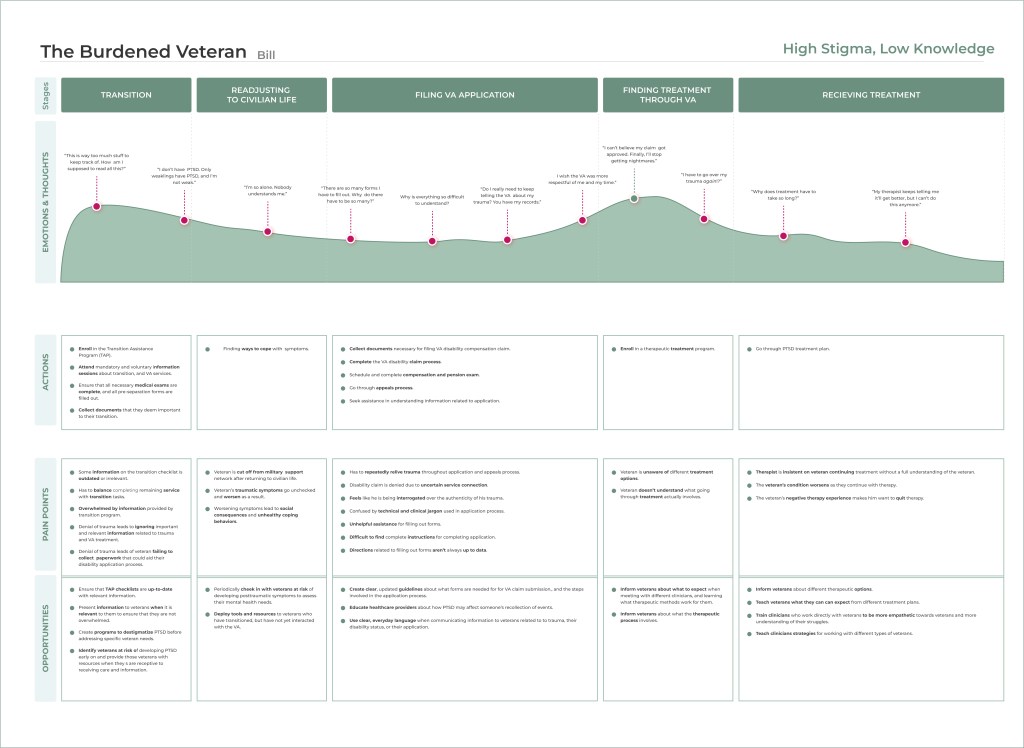
Journey mapping revealed the following insights:
- Bill’s stigmatized beliefs prevent him from being receptive to helpful information.
- Bill struggles to understand the overwhelming amount of information needed to go through the system.
- Bill’s high expectations for treatment are caused by insufficient information, which increases stress.
- A lack of understanding and empathy from clinicians worsens Bill’s condition.
Skills Learned
This project allowed me to showcase many of the design and research skills I had gained not only through this program, but through my psychology Master program as well. Moreso, it allowed me to develop identity-affirming interventions that pulled concepts from HCI to benefit a vulnerable community. It showed me how I can use my skills and experience to not only talk about trauma, but to put my knowledge into practice as well.